- Plastic Surgery
- Liposuction
- MedSpa
- Patients Gallery
- Our Practice
- Resources
- Contact

- The Stigma and Strain of Large Breasts
- Breast Reduction Surgery Was “One of the Best Decisions I Ever Made”
- Teenage Breast Reduction Benefits
- Should I Wait to Have Plastic Surgery?
- Will Insurance Cover My Breast Reduction Procedure?
- Scientific Evidence for the Benefits of Breast Reduction Surgery in Young Women
- Breast Reduction with Lollipop Technique: Shorter Scar and Recovery Time
- Schedule a Consultation
Uncomfortably large breasts can ignite an overwhelming sense of insecurity for adolescent young women. Fortunately, breast reduction surgery can have significant benefits for teenagers suffering from the physical symptoms and emotional toll of having overly large breasts.
The Stigma and Strain of Large Breasts
The stigma that a young woman experiences when her breasts are disproportionally large interferes with her body image and sense of confidence. Physically, there is daily discomfort from the strain on the neck, back, and shoulders. Socially, young people with large breast growth can experience harassment, teasing, and other harmful things in various social spaces in their lives.
Breast Reduction Surgery Was “One of the Best Decisions I Ever Made”
This is the story of one teenager’s experience with uncomfortably large breasts, beginning at age 11:
“In the fourth grade I began wearing a bra; by sixth grade I was wearing a C cup. It was hard for me to look around and wonder why no one else looked like I did. By seventh grade being different bothered me so I wore a jacket and never ever took it off. I was a D cup and I started getting back pain. I really didn’t ever think about getting [plastic] surgery until I was a freshman in high school. Believe me, I had to argue with my parents a ton. I was always getting back massages and people constantly made sly comments on the side.
“By 10th grade, I was a DD and all my problems seemed to escalate. I was going to my chiropractor once a week for about a year and a half. Finally, I guess my parents got sick of me complaining about my back pain and how miserable I was and they decided to let me look into surgery.
Worries and Hurdles
“There were a lot of decisions that my family and I had to make. Would I regret it? Do I really want this? Will I change my mind at some point? How long would recovery be? With any surgery, of course you are going to have to have recovery time. I have never had an easier recovery than with this surgery.
“It was very easy. I even did it during the school year. After four days, the weekend included—so basically, two missed days of school—I was back at school doing normal things.
No Regrets
“I have absolutely no regrets about having this surgery at age 17. I look and feel so much better. My back pain went away almost immediately, which was a huge relief. I am really happy with it and I think that it was one of the best decisions that I have ever made.”
Teenage Breast Reduction Benefits
Once the breasts are reduced to be in proportion with the rest of the body, a more normal body image can develop, and social interactions become more comfortable. These young people often feel “abnormal” and have a desire to “be normal.” The results are immediate and the benefits of this surgical procedure last a lifetime.
Should I Wait to Have Plastic Surgery?
It is important to know that not all teenagers are candidates for surgery. Undergoing breast reductions requires a level of maturity and a certain stage of physical development. Breast surgery should be performed only when the breasts are fully developed, as postoperative breast growth could alter the benefits of the procedure. There is also the recovery period to think about and the permanently altered physical appearance.
Unfortunately, many young patients are told, incorrectly, to wait until they are older to undergo breast reduction surgery, not because they are not mature enough, but because of a medical bias in some plastic surgeons that teenagers should not have plastic surgery. Nothing could be more unfounded. Teens who have had breast reduction surgery consistently wish they had done it sooner.
Will Insurance Cover My Breast Reduction Procedure?
Every woman with discomfort from overly large breasts knows how much of a disability there is from daily neck, back, and shoulder pain and strain. And every patient who has had a breast reduction experiences immediate relief in the recovery room. So why do insurance companies have complex rules and protocols to avoid “paying” for a breast reduction surgery?
Dr. Ditesheim says, as a doctor and surgeon, his first concern is for his patients – their health and wellbeing. For more information, here is information from the medical literature that explains the history of breast reduction insurance payment and validates the significant benefit of breast reduction surgery, especially for young women.
There is an Arbitrary “Cut-Off” for Breast Resection Weight
Paul Schnur, a well-respected plastic surgeon, published a study in the Annals of Plastic Surgery (APS) in 1991 titled “Reduction Mammoplasty: Cosmetic or Reconstructive Procedure?” (1). This study was not designed to predict the amount of tissue to be removed, but rather to provide a cutoff for the insurance companies to determine medical necessity for breast reductions.
This study did not use a validated questionnaire that looked at how patients functioned after the surgery, nor did it take into account other parameters such as age, density of breast tissue, or body mass index. Despite its limitations, insurance companies are still relying on the Schnur scale to guide reimbursement of reduction mammoplasties over three decades later.
Insurance Company Criteria Is Not Validated with Current Medical Literature
The Schnur scale has been studied and found to have a low predictive value. Today, better models exist and have been published using a validated questionnaire (Breast-Q). These studies are prospective ( looking at how women rated their disability before and after the surgery), tend to focus on younger patients (under 25), evaluate different models of health outcomes to see if current criteria are still validated, and follow women for up to 21 years.
All these studies asked the question “Does breast reduction surgery provide a functional improvement in quality of life, psychosocial functioning, self-esteem, bodily pain, and breast-related symptoms?” In each of these studies, there was strong evidence that breast reduction surgery has a significant functional benefit and resection weight does not correlate with the degree of symptomatic relief after reduction mammoplasty.
What is Breast-Q and Why is it Important?
The Breast-Q is a validated condition-specific patient-reported outcome instrument. This instrument is the most precise tool to measure the impact of a health condition and the success of surgical intervention from the patient’s perspective.
Scientific Evidence for the Benefits of Breast Reduction Surgery in Young Women
One study followed 37 women with a median age of 20 years for a median follow-up of 21 years. This was a retrospective study using the Breast-Q questionnaire post-operatively. The conclusion: “Young reduction mammaplasty patients experience excellent breast-related quality of life decades after surgery” (2). They found that neither the age at time of surgery, amount of excess breast tissue removed, or body mass index affect the quality of the results.
Another study followed 512 young women for up to 7 years after their procedures to determine the benefits of reduction mammoplasty. They noted that 80% of women had been symptomatic since their teens, despite being told to either wait or not to have surgery for relief of symptoms. Once again, this study confirmed that reduction mammaplasty demonstrated “gains in physical well-being, bodily pain, psychosocial functioning, self-esteem, and breast-related symptoms.” (3)
Is the Functional Benefit of Reduction Mammaplasty Dependent on the Amount of Tissue Removed?
132 Australian women were studied before and one year after a breast reduction using the Breast-Q questionnaire. Marked improvement in health-related quality of life was experienced by patients regardless of age, body mass index, or minimum amount of tissue removed.
This is the largest prospective study to date using a validated questionnaire model. This study “supports previous findings that there is no evidence or rationale to justify any policy that restricts funding for reduction mammaplasty based on arbitrary cutoffs for body mass index or a minimum weight of resection”. (5)
How Do Women with Breast Hypertrophy Compare to “Normal” Women Before and After Surgery?
The study above showed that “breast hypertrophy represented a significant health impairment to women, with preoperative scores significantly lower in all areas of satisfaction and health-related quality of life. At one year after the breast reduction procedure, scores increased significantly across all Breast-Q scales to levels at least equivalent to the norm.” This demonstrates the long-term benefit and success of breast reduction surgery in bringing satisfaction and quality of life to women in general.
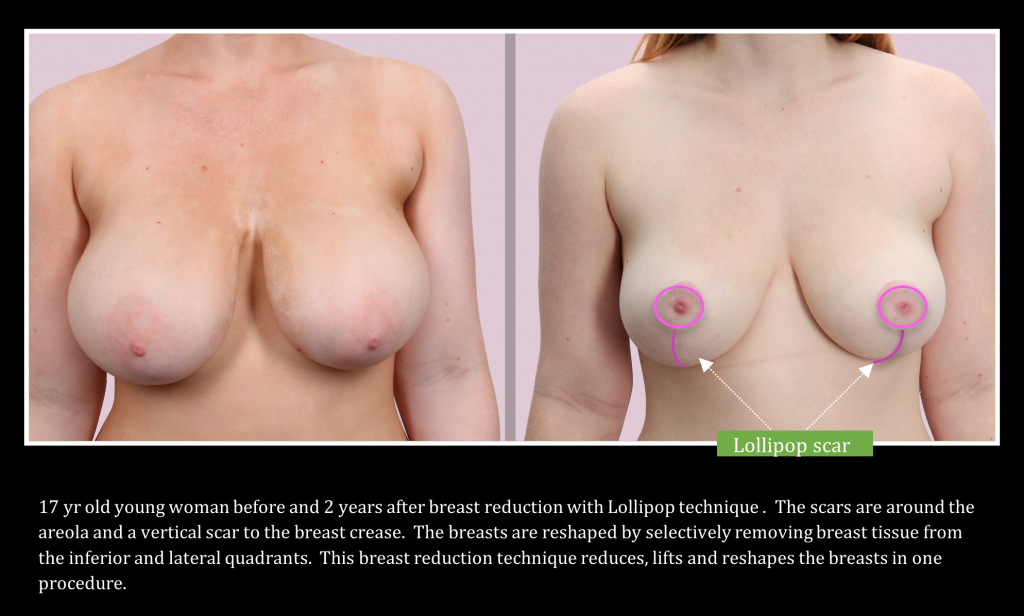
Breast Reduction with Lollipop Technique: Shorter Scar and Recovery Time
While all breast reduction techniques reduce breast size, the new “lollipop” technique, so-called because of the lollipop shape of the scar, reduces the breast with a much smaller scar, a better breast shape, and a shorter recovery. Creating the most “normal” breast requires a smaller size, a natural shape, and the least noticeable scars.
Schedule a Consultation
Dr. Jeffrey Ditesheim is more than a board-certified plastic surgeon. He is a sensitive and experienced professional whose focus is always to help his patients feel more beautiful and confident. Schedule a consultation with Dr. Ditesheim to learn more about breast reduction surgery and whether it’s the right time and the right surgery for you.
References:
- Schnur PL, Hoehn JG, Ilstrup DM, Cahoy MJ, Chu CP. Reduction mammaplasty: Cosmetic or reconstructive procedure? Ann Plast Surg. 1991;27:232-237.
- Krucoff KB, Carlson AR, Shammas RL, Mundy LR, Lee HJ, Georgiade GS. Breast-related Quality of Life in Young Reduction Mammaplasty Patients: A Long-Term Follow-up Using the Breast-Q . Plastic and Reconstructive Surgery. 2019; 144:743e-750e.
- Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and Quality of Life following Reduction Mammaplasty in Adolescents and Young Women. Plastic and Reconstructive Surgery. 2019; 144:572-581.
- Boukovalas S, Padilla PL, Spratt H, Tran JP, Li RT, Boson AL, Howland N, Phillips LG. Redefining the Role of Resection Weight Prediction in Reduction Mammaplasty and Breaking the “One-Scale-Fite-All” Paradigm. 2019; 144:18e-27e.
- Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of Breast Reduction Surgery Using the Breast-Q: A Prospective Study and Comparison with Normative Data. 2019; 144:1034-1044.


 (704) 542-8686
(704) 542-8686